Three hundred seventy-four plasma specimens were taken from patients within the first month following they were identified with SARS-CoV-2 illness, and the specimens were tested for SARS-CoV-2 blood and single lymphocytes. The study looked at 1,387 metabolomic proteins as well as 1,050 blood chemicals.
Experts in different branches of medical science try to find alternatives with the help of which it can be possible to find the cause and probabilities for one to be a victim of this virus and as a result, they have to the metabolic alteration to indicate the same.
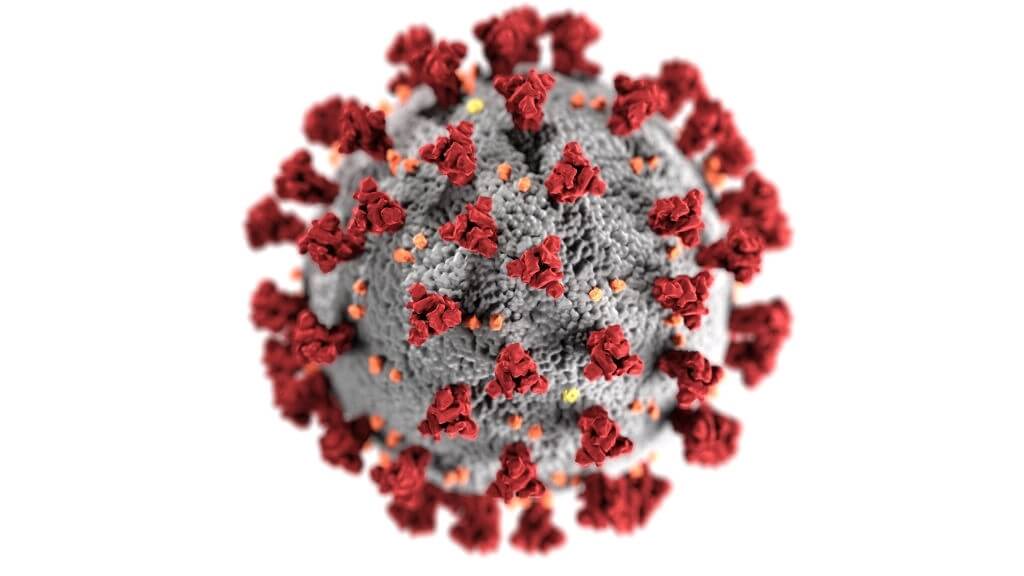
COVID Associated Metabolic Alterations Plasma And Immune Cells Can Predict Patient Survival
“We know that there is a range of immune responses to COVID-19, and the biological processes underlying those responses are not well understood,” said co-first author Jihoon Lee, a graduate student at Fred Hutchinson Cancer Research Center.
“We analyzed thousands of biological markers linked to metabolic pathways that underlie the immune system and found some clues as to what immune-metabolic changes may be pivotal in severe disease. We hope that these observations of immune function will help others piece together the body’s response to COVID-19. The deeper understanding gained here may eventually lead to better therapies that can more precisely target the most problematic immune or metabolic changes.”
COVID-19 individuals have a variety of immunological responses, which can result in silent SARS-CoV-2 infection or death. Scientists discovered fundamental biochemical alterations that influence how lymphocytes respond to the illness after analyzing samples of blood from almost 200 COVID-19 participants. These alterations are linked to the intensity of the illness and may be utilized to forecast the survival of patients. The study’s results are reported in Natural Biotech.
“We have found metabolic reprogramming that is highly specific to individual immune cell classes (e.g. “killer” CD8+ T cells, “helper” CD4+ T cells, antibody-secreting B cells, etc.) and even cell subtypes, and the complex metabolic reprogramming of the immune system is associated with the plasma global metabolome and are predictive of disease severity and even patient death,” said co-first and co-corresponding author Dr. Yapeng Su, a research scientist at Institute for Systems Biology.
“Such deep and clinically relevant insights on sophisticated metabolic reprogramming within our heterogeneous immune systems are otherwise impossible to gain without advanced single-cell multi-omic analysis.”
The researchers observed that increasing COVID-19 severity is connected with chemical abnormalities in human plasma, indicating enhanced night invulnerable activities. Moreover, scientists found that each main innate immune subtype has various metabolic signatures, which they discovered by single-cell genomics.
“This work provides significant insights for developing more effective treatments against COVID-19. It also represents a major technological hurdle,” said Dr. Jim Heath, president and professor of ISB and co-corresponding author on the paper. “Many of the data sets that are collected from these patients tend to measure very different aspects of the disease and are analyzed in isolation.
Of course, one would like these different views to contribute to an overall picture of the patient. The approach described here allows for the sum of the different data sets to be much greater than the parts, and provides for a much richer interpretation of the disease.”
Researchers from ISB, Stanford University’s Fred Hutchinson Cancer Research Center, the University of Washington, and the Howard Hughes Medical Institute collaborated on the study.
We’re barely scratching the surface of host variables like the different transcription of cell-surface receptors, which could influence infection susceptibility, illness appearance, and consequences.
The emergence of tissues and stage-specific variables that contribute to disease will lead to the development of innovative, efficient, and illness treatment methods that regulate the reproduction of the viral and reducing inflammation harm until vaccines are accessible.