In a report published today in Nature Medicine, researchers from the University of Pittsburgh School of Medicine demonstrate that neuroinflammation is a critical driver of the development of pathologically misfolded proteins in the brain, which causes cognitive impairment in Alzheimer’s disease patients.
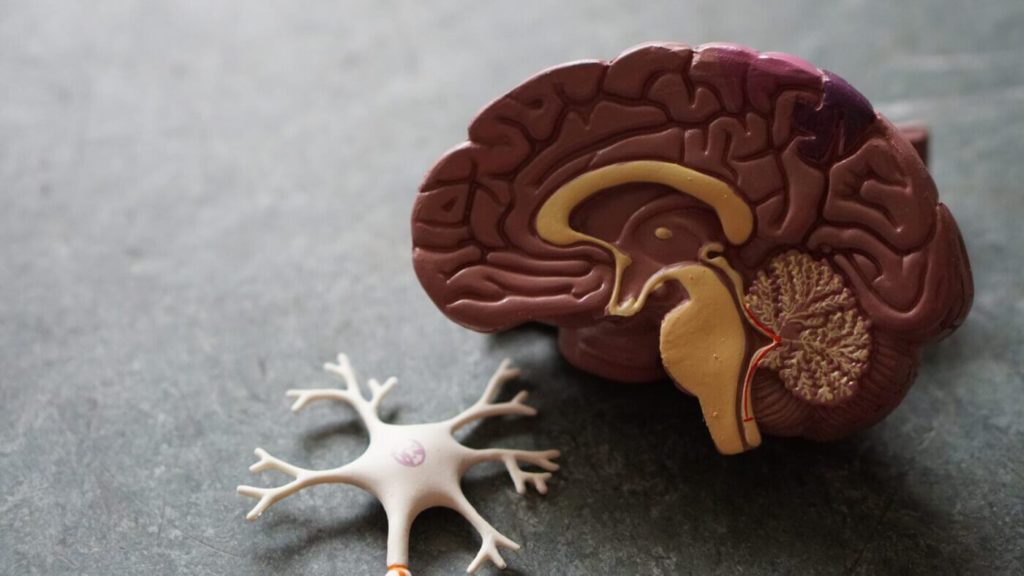
The researchers demonstrated in real patients for the first time that neuroinflammation—the activation of the brain’s indigenous immune cells, termed microglial cells—is not only a side effect of illness progression, but rather a critical upstream process required for disease development.
How Brain Tissue Inflammation Plays A Major Role In Alzheimer’s Disease Progression
The identification of this element can help the experts prepare a course of action that can control the tissue inflammation in the brain that can be an important factor for Alzheimer’s.
This can be tested with some present tests in the market and in case of any inflammation found on such tissues it can be addressed on an urgent basis.
This can help one prevent Alzheimer’s in a long run. Some more analysis is being done and this research may offer some more surprises mentioned by an expert.
Lead author Tharick Pascoal, M.D., Ph.D., assistant professor of psychiatry and neurology at Pitt, stated, “As a young resident neurologist in my native country of Brazil, I saw that many patients with Alzheimer’s disease are neglected and without access to adequate care.”
“Our findings imply that treating both amyloid plaque development and neuroinflammation in combination may be more successful than treating either disease alone.”
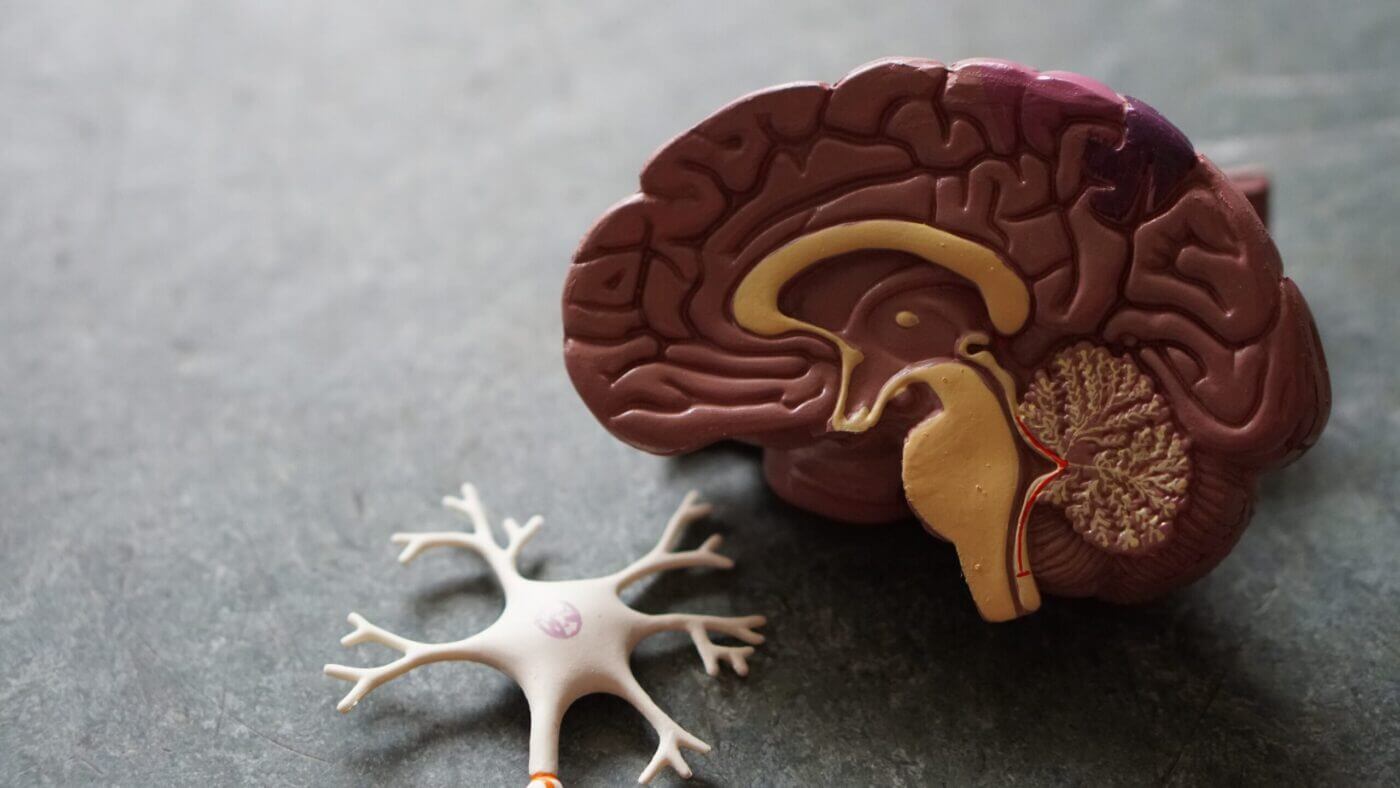
Alzheimer’s disease is marked by the formation of amyloid plaques, which are protein aggregates trapped between nerve cells in the brain, and tau tangles, which are clumps of disordered protein fibers that form inside the nerve cells.
Although there is considerable evidence that microglial activation causes the growth of tau fibers in Alzheimer’s disease in cultured cells and lab animals, this mechanism has never been confirmed in people.
The findings of the study imply that addressing neuroinflammation might be useful for patients with early-stage Alzheimer’s disease, since it could help reverse or at least delay the buildup of pathologic tau protein in the brain, preventing dementia.
The researchers utilized live imaging to peer deep into the brains of persons with various stages of Alzheimer’s disease and healthy aging adults to identify the process by which disorderly tangles of tau protein fibers and amyloid plaques spread across the brain and contribute to dementia.
Neuroinflammation was shown to be more frequent in older persons, and it was much more prominent in patients with moderate cognitive deficits and Alzheimer’s disease-associated dementia.
Using bioinformatics, it was established that tau propagation was dependent on microglial activation. This is a crucial factor that relates the consequences of amyloid plaque aggregation to tau spread and, eventually, cognitive impairment and dementia.
“Amyloid plaques are found in many old people’s brains, but they never acquire Alzheimer’s disease,” Pascoal added. “We know that amyloid buildup alone does not cause dementia; nevertheless, the findings imply that the combination between neuroinflammation and amyloid pathology is what triggers tau propagation and finally leads to widespread brain damage and cognitive impairment.”
There are many other research projects underway, but the findings are yet to be published. Further research on the same field is bound to produce better insights that might revolutionize the medical industry forever.
The senior and co-corresponding author of this article is Pedro Rosa-Neto, M.D., Ph.D., of McGill University. McGill University, the University of Gothenburg in Sweden, the University of Antwerp in Belgium, the University of Toronto in Canada, and Imperial College London are among the other writers. The efforts of these scientists helped me understand Alzheimer’s like never.