Unfazed, stem cell researchers, cell scientists, communicable diseases specialists, and cardiac surgeons from the University of California San Diego Medical school banded together to explore whether they could conquer various challenges.
Researchers had failed to develop lab analogs of SARS-CoV-2 infections, the lung virus causes COVID-19 since the epidemic hit the US in early 2020. Animal studies have succeeded in the past, and efforts to develop mature human lungs have flopped in the past since not all types of cells persisted.
Remarkable Achievement But Yet Need More: Human Mini-Lungs Grown In Lab
“This human disease model will now allow us to test drug efficacy and toxicity, and reject ineffective compounds early in the process, at ‘Phase 0,’ before human clinical trials begin,” said Pradipta Ghosh, MD, professor, director of the Institute for Network Medicine, and executive director of the HUMANOID Center of Research Excellence (CoRE) at UC San Diego School of Medicine.
Soumita Das, Ph.D., associate professor of pathology at UC San Diego School of Medicine and founding co-director and chief scientific officer of HUMANOID CoRE, co-led the study with Ghosh.
According to experts, it is a remarkable achievement even if it is a small part as it may open the gates for further development in this field, and tomorrow we can see the development of more human organs also.
This can help mankind in many ways. Presently the developed part is also under research and more improvement will be made in coming days said a team member that has got this achievement while explaining to the media.
The scientists revealed that the higher airways neurons are required is for influenza to initiate infections, whereas the bottom airways cells are essential for the inflammatory system, by infecting the lungs spheroids with SARS-CoV-2. These cell types have a role in the overactive immune reaction known as a cytokine flood, which has been seen in acute COVID-19 instances.
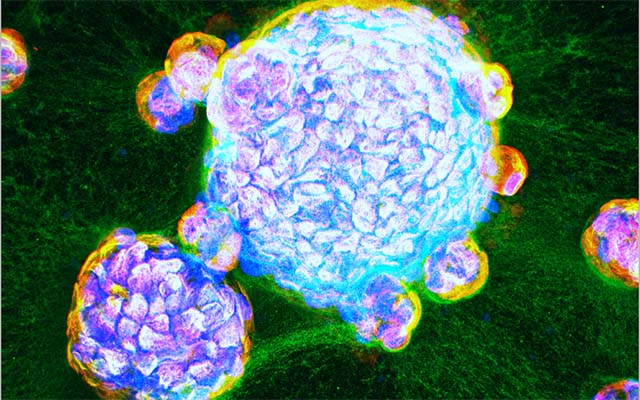
Human stem cells taken from lung tissue that was resected owing to lung disease were grown repeatable by cell therapy researchers just at HUMANOID CoRE, lead by Das. They are capable of maintaining cells that line both the top and bottom passages of lung tissue, especially specialist alveolar cells designated as AT2, using a specific cocktail of tissue factors.
The lungs spheroids acted like real-world lungs, not whether they were infected with SARS-CoV-2. The scientists demonstrated that their mature lung spheroids reproduced COVID-19 more than any other contemporary lab model in head-to-head assessments using the same yardstick (transcriptomic patterns).
Other models, such as fetal throat organoids or designs that rely solely on airway obstruction cells, allow for viral illness but no immune system.
“Our lung organoids are now ready to use to explore the uncharted territory of COVID-19, including post-COVID complications, such as lung fibrosis,” Das said. “We have already begun to test drugs for their ability to control viral infection—from entry to replication to spread—the runaway immune response that is so often fatal, and lung fibrosis.”
“Because our HUMANOID CoRE lung organoids are scalable, personalized, propagatable, and cost-effective, they are quite unlike any other existing model,” said Ghosh. “This is a significant advance that can enable the modeling of lung diseases and pandemics beyond COVID-19.
In fact, other academic and industry partners are already beginning to use these organoids in disease modeling and drug discovery. This is when I feel that translational research is immediately transformative.”
The group thinks that effective treatment ideas can be quickly pushed to medical studies since their results in humans cells in vitro are more certain to be applicable to human cancer than discoveries in mouse models or cell lines.