Researchers have presented a new view of the causes of sepsis, which is sometimes lethal when the infection spreads across the body. Leakage of the blood vessels can indeed induce sepsis instead of a symptom as assumed earlier.
Sepsis is the second biggest cause of mortality in acute care facilities, killing around 1,400 people per day worldwide. The fatality rate is still high, between 30 to 50%, despite intensive research. Treatments consist mostly of surgical removal or discharge, antibiotics, and supportive care of the contaminated location.
A New Study Found That Sepsis Therapeutics Makes Blood Vessels Leaky
Looking at the death rate and people suffer from Sepsis this research holds great significance. With the help of the same now it is possible to find the area and prevent other leaks from the vein with different options that can help improve the health of the patient.
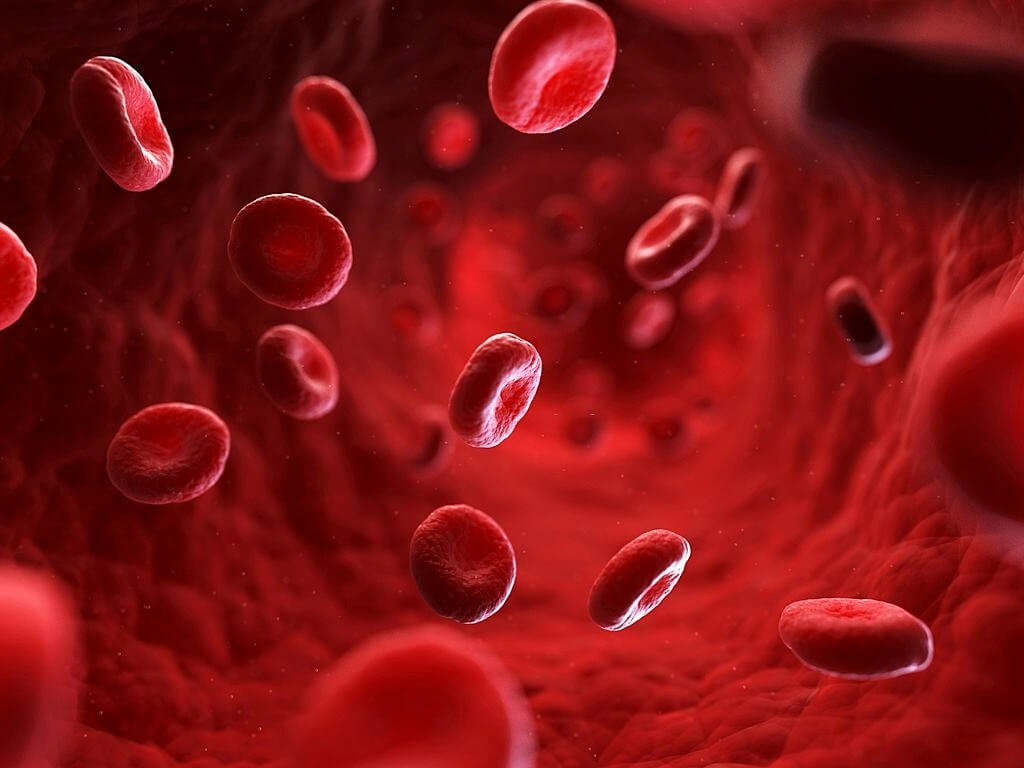
Sepsis develops if the body fights hard to combat an infection, which damages the patient’s inner tissues as collateral damage to the over-activated immune system.
This can make blood vessels leak and prevent large bodies from getting the oxygen and nutrition they need to sustain their lives. Sepsis is a primary reason for ending up in the critical care unit, many of whom suffer from COVID-19. It’s notoriously difficult to deal with the condition when there are no medicines that can help stabilize the blood vessel cell membrane.
San Diego Medical School is focusing on how to best manage how the body maintains the permeability of blood vessels and how they would intervene during periods of sepsis, injury, or other situations to restore the stability of the blood vessel.
An HSP27 protein has recently been found to be a part of regulating the leakage of blood vessels. Cells add and then remove chemical tags on HSP27 to aid dissolve or increase the blood vascular barrier.
Barriers to the blood vessel must be dynamic—permeable to press immune cells out so that they get to the site of the infection. HSP27 is linked to proteins that contribute to the forming of the cell’s “skeleton,” as per Trejo. This is why HSP27 can influence the permeability of blood vessels—fortifying the barrier skeleton of cells.
Trejo has extensively examined G-protein-coupled receptors, proteins that are entrenched all through the body in cell membranes, where they operate as signal transducers that enable cells to react to their surrounding environment. For most biological functions, GPCRs play a significant role. About one-third of all therapeutic medicines on the market are working because GPCR signals are affected.
The fact that the majority of GPCRs work as master regulators and affect a number of distinct cell processes is one difficulty in treating a disease. Halting a GPCR can have several undesirable outcomes.
Trejo’s team hopes to enable the development of more accurately blood vessel-stabilizing medications that have less unwanted side effects, by focussing further downstream—not on master’s GPCR, but on particular targets, such as HSP27—to help.
According to Trejo, “It’s become apparent that you can develop different molecules that can bind to receptor and ‘bias’ them—make them signal in a very specific way to some pathways but not others. “He added, “It’s what we call biased agonism, and it’s a huge advantage for drug development. It means we can develop not just an on/off switch, but a drug that can switch a receptor ‘off’ or eight different types of ‘on.’ We want to be able to tweak which pathways are on and not touch others.”
The team is planning to examine additional cells that assist blood arteries to resist injury as well as inflammation.