Only a small percentage of the peptides discovered are known to be released via exocytosis, implying that gastric secretion happens through various processes.
Major vault protein specified in the relevant two of the reported protective proteins were not found in the fluid from human epithelial cultures or nasal or bronchoalveolar lavage.
How Mucus Protein Contributes To The Progression Of COPD, Asthma, & Other Lung Diseases
Further exome sequencing of pure glandular mucus could shed light on how normal airways keep their surroundings clean. Mucus is an outermost covering of gel-like liquid that coats our airways and is made up primarily of proteins called mucins.
One of these, MUC5B, is essential for our body’s natural defenses against the numerous substances we inhale. However, another mucin known as MUC5AC swells excessively in response to cigarette smoke and allergens, compounding health issues.
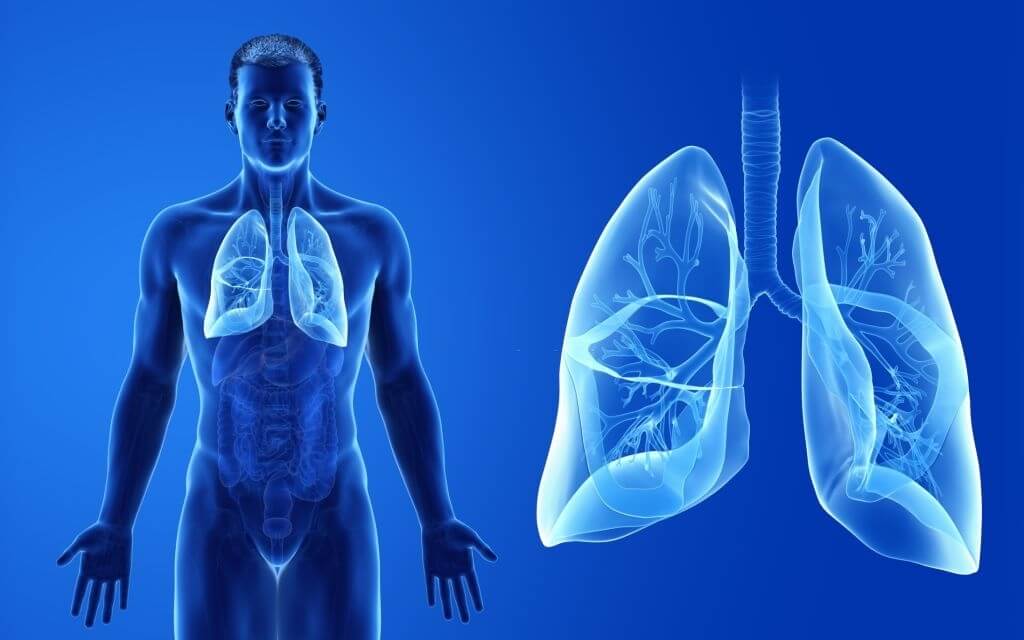
For the first time, researchers at the University Of North Carolina School Of Medicine have revealed how MUC5AC disrupts the airways of people suffering from respiratory diseases, including COPD and asthma. We may only notice mucus when there is an excessive amount of it, such as when we have a cold, and the seeming overproduction of mucus is the body’s natural response to a virus.
However, mucus layers throughout the body are essential for good health, and the mucin proteins that produce mucus, mucus are essential as well. The requirements specification of each surface, commonly known as the epithelium, determines the mucin composition of mucus lining distinct surfaces.
The body needs different nutrients to keep it fit, strong, and healthy, and among all such elements, protein is the most significant one. The mucus is also formed with one of the types of protein, but it has several impacts on other elements as well.
Surprisingly this can lead to severe medical conditions, including cancer, asthma, and issues with the lungs. Accumulation of mucus can lead to tough conditions for one, and only protein can be held responsible for this. If the level of protein is controlled in mucus, it may not have a dangerous effect on different organs, and life can be saved.
For example, the mucin MUC2 has been altered to form a “tight mucus layer” in the small intestine and colon, providing a niche for microbes while protecting the underlying epithelium against bacterial invasion.
MUC6 and MUC5AC work together in the stomach to form a barrier that protects the epithelium from the damaging effects of excessive acidity.
Saliva protects the mouth, which is a significant portal for food and microorganisms, and MUC5B is the most common gel-forming mucin.
MUC5B and MUC5AC are expressed in different ways throughout the respiratory system, depending on each portion of this complicated system.
MUC5B, which has been proven crucial for innate lung defense, is secreted by glands beneath the mucous membrane. Meanwhile, MUC5AC is secreted mostly by surface cells in the larger airways.
On the other hand, small airways begin to release MUC5AC in response to persistent stressors like cigarette smoke and allergens. As Kesimer and colleagues recently showed in the Lancet Respiratory Medicine, MUC5AC is intimately linked to the incidence and development of chronic obstructive lung illnesses, such as chronic bronchitis and COPD.
In the PNAS publication, Kesimer and co-authors discuss many ways they employed to better understand the molecular features of these two glycans, namely how MUC5AC gets stickier and splits into static, tethered mucus networks seen in chronic airway health issues.
MUC5AC binds much more to surfaces that generally reject liquids, such as the surfaces in airways, and MUC5AC generates stiffer layers that are thicker and more elastic than layers that include MUC5B prominently according to Kesimer’s research.