The study was reported in Genes & Development and was funded by National Institutes for Health. UT Southwestern is one of the best 25 institutions in the country for diabetic & endocrine treatment.
“It’s like flipping a switch. We removed the ‘brake’ on the energy-burning pathway in fat cells by engineering a mutation that disrupts the interaction between a single pair of proteins,” said study leader Rana Gupta, Ph.D., Associate Professor of Internal Medicine. “Our research demonstrates that releasing this brake in fat cells can potentially help make existing diabetes medications much more effective.”
Change Storing Fat Cells Into Energy-Burning Fat Cells
Obesity is the number one enemy of human health, and in the USA, only millions of people suffer from obesity. With the help of this study, one can find ways to have reduced fat in the body that can lead to a fit and well-shaped body over a period, said an expert.
The Touchstone Diabetic Institute at UT Southwestern Medical Center has effectively employed CRISPR genome modification to convert fat cells that are ordinarily utilized for preservation into energy-burning neurons.
“There is tremendous interest in driving the production of these energy-burning fat cells as a treatment against metabolic diseases such as diabetes,” said Dr. Gupta, who called obesity “the pandemic before the pandemic.”
Overweight incidence in the United States climbed from 30.5 percent to 42.4 percent between 1999 to 2018, as per the Centers for Disease Control and Management, with more of those affected suffering from diabetes as a result. Upwards of 30 percent of People today have diabetes, with American Diabetes Association estimating that another 18 percent of the population is diagnosed or has prediabetes. The expense is staggering: documented diabetic care costs $327 billion each year, or nearly $1 for each $7 spends on health treatment in the United States.
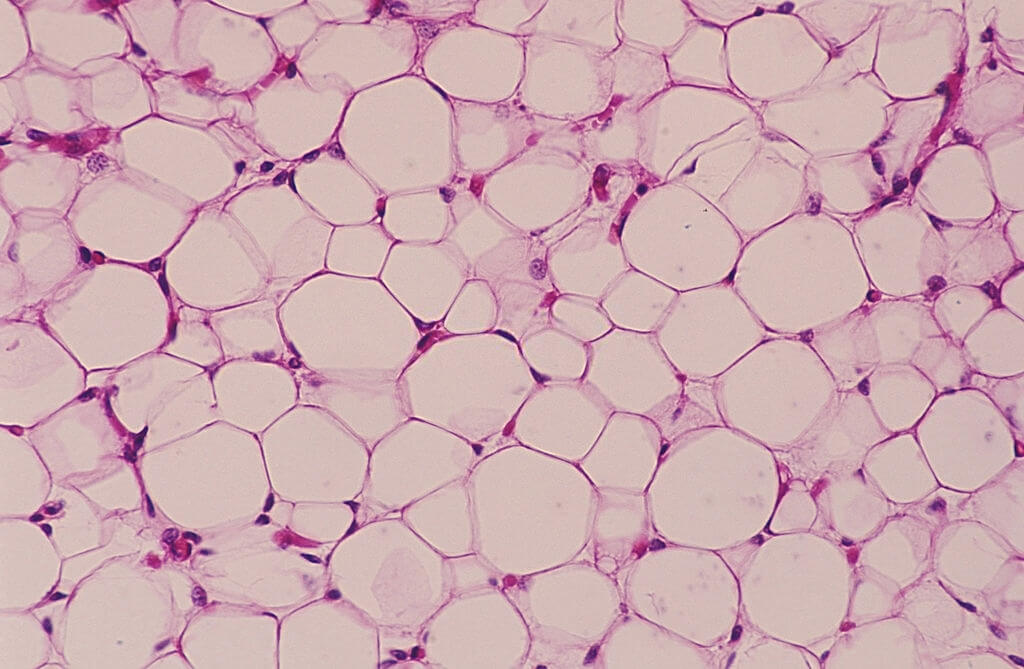
Individuals have two kinds of fat cells: white cells, which store calories and grow in quantity and volume in obese individuals, and energy-burning brown or dark cells, which consume extra calories to generate warmth and boost energy expenditures. Brown fat cells are also protective against the formation of diabetes and heart illness. Obese individuals have considerably fewer brown or dark fat cells, according to Dr. Gupta.
From 2006, Dr. Gupta had started researching fat cells & metabolic disorders. In 2012, he joined the faculty at UT Southwestern, where his group uses cutting-edge genomic information & molecular/cellular biology to investigate many facets of adipose tissue (fat cell) formation.
Overweight & obesity-related disorders like Type 2 diabetes, heart events, and cancers are all linked to fat tissue dispersion and malfunction. According to Dr. Gupta, the expanding overweight pandemic and increasing expenses involved with managing metabolic disorders have heightened the need to know all elements of adipose biochemistry, particularly where fat cells originate across the system.
Dr. Gupta and his colleagues published a recent report in Cell Metabolism in 2016 that was partially supported by the National Institutes of Health.
Brown & beige adipose cells have a tremendous ability to turn energy to temperature, which could open up new treatment avenues for metabolic disorders, including overweight and type 2 diabetes, which is on the rise. To catabolize fats and oils & glucose, such as thermogenic lipids, use mitochondria phosphorylation that untangles the respiratory, resulting in a rise in energetic consumption.
A variety of noncanonical ways demonstrates the thermogenic ability of beige adipocytes that originate in adipose tissues. This study will present a broad overview of thermogenic adipose, with a focus on UCP1-independent adaptation materials are converted and developing processes of “being,” that could give further support for addressing thermal fat to treat obese as well as other metabolism problems in people.