As per a big study published at a medical conference, individuals who suffer from ovarian, pancreatic, & some additional kinds of cancers may live longer if administered an anti-nausea medicine following the operation. Scientists discovered that almost over three times as numerous individuals who would not get dexamethasone perished three months following their major surgery as individuals who received.
This treatment can help them keep common diseases away and have better living even at an old age. The recent survey is conducted by a team of experts where several factors of such diseases are taken into account in correlation with patients’ medical conditions from different regions and different age groups. The team collected the samples from vast data to understand the general effects on this patient group.
Anti-Nausea Medication May Assist Some Cancer Patients
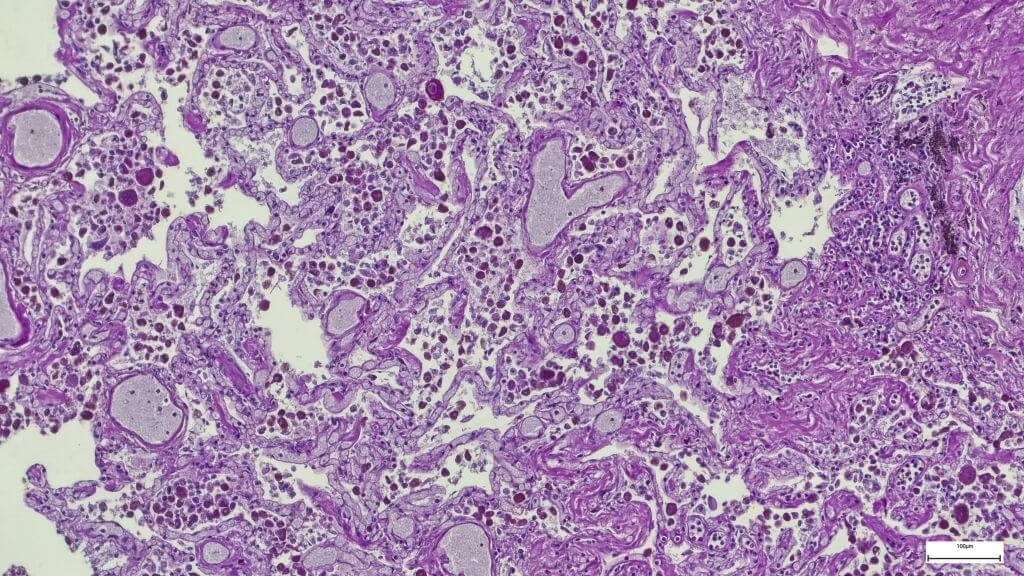
Individuals are administered dexamethasone to reduce nausea following operation and throughout chemo. Scientists discovered that dexamethasone could help individuals having non-immunogenic tumors such osteosarcoma and malignancies of the chest, uterine, ovary, esophagus, pancreatic, thyroid, bone, and knees enhance their middle- to brief results.
“Dexamethasone has positive and negative effects it inhibits cancer growth, but also suppresses the immune system,” said Maximilian Schaefer, M.D., Ph.D., senior author of the study and director of the Center for Anesthesia Research Excellence. “Previous research has reported that in cancers in which the immune system controls cancer growth, the positive and negative effects of dexamethasone balance each other, so there is no benefit. Ours is the first large study to show that for a wide variety of cancers where the immune system does not play a major role, the positive effects seem to predominate.”
Scientists examined the data of 74,058 individuals who have non-immunogenic malignant tumors removed at Deaconess Medical Center and Massachusetts General Hospital in Boston from 2005 and 2020. Dexamethasone was given to 25,178 (34 percent) of the participants throughout the operation. Following three months, 209 (0.83 percent) of those who took dexamethasone perished, compared to 1,543 (3.2 percent) of those who received not.
Even when accounting for a variety of circumstances, such as the reality of dexamethasone is frequently given to young individuals, individuals who got it to have a 21 percent lower chance of death after a year following operation. Dexamethasone was found to be especially effective for individuals with malignancies of the ovarian, uterine, or cervical in a subsequent study.
“Based on our data, physician anesthesiologists should feel more confident in administering dexamethasone to patients undergoing surgery for non-immunogenic cancers,” said Dr. Schaefer. “It not only helps with nausea, but it also may result in improved survival.”
Neither incident studies & exact conditions were found in a prior systematic evaluation of haloperidol within this situation. Just case reports are identified to justify the usage of haloperidol in a literature evaluation on antiemetics in the management of nausea in late malignancy patients. According to a consensual evaluation of the treatment of vomiting and diarrhea in persons with cancers & other persistent conditions, haloperidol is “likely to be useful.” Furthermore, many consider haloperidol may be among four key medications for the treatment of end-of-life problems.
We detected RCTs of haloperidol for postoperative sickness & vomit, intestinal issues, and prophylaxis of stomach pain linked to radiation therapy and chemotherapy while not thoroughly reviewing the information in additional situations. According to a meta-analysis, the quantity required to treatment for a favorable outcome to avoid surgical upset stomach when contrasted to placebo. While such research may serve to educate practice, it is unclear to what degree they are useful to the hospice care population. In pain management, the reasons and processes of nausea could be varied. This could influence the treatment effect.