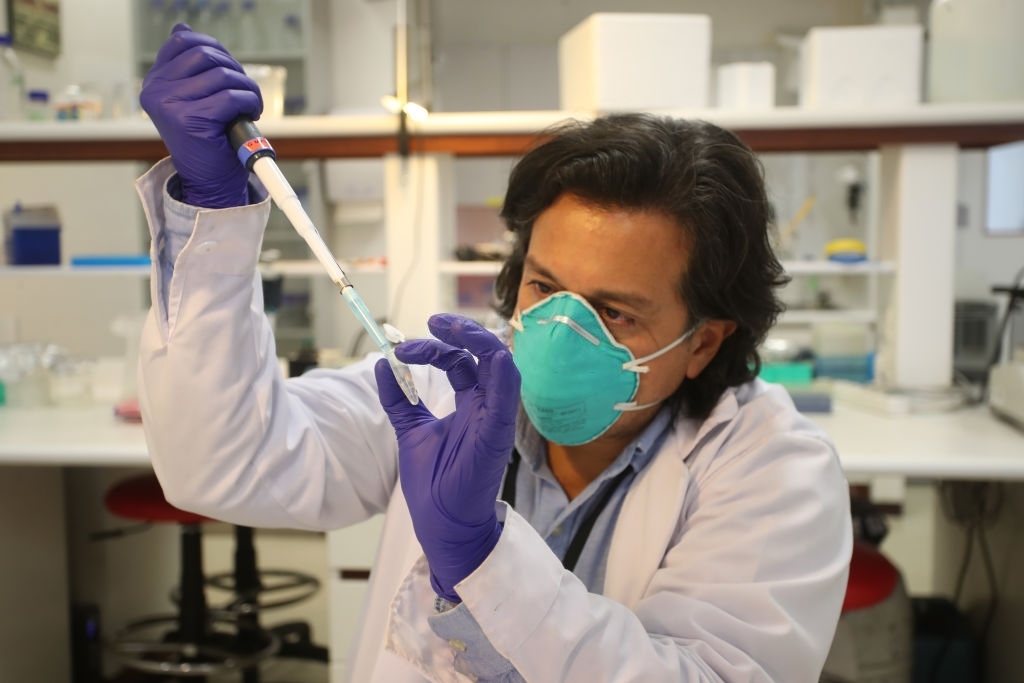
A new method for delivering molecular medicines to cells has been created by researchers from MIT, the McGovern Institute for Brain Research at MIT, the Howard Hughes Medical Institute, and the Broad Institute of MIT and Harvard.
Human Protein Is Being Used To Deliver Molecular Medications To Cells
SEND (Selective Endogenous eNcapsidation for cellular Delivery) is a technology that may be configured to encapsulate and distribute various RNA contents. SEND uses the body’s endogenous proteins to produce virus-like fragments and bind RNA, but it may elicit a lower immune reaction than alternative delivery methods.
As per an expert, the cells can be improved with their condition with the help of this protein and hence they can be more effective in handling various infections or viral attacks. The molecular medication affects the health of cells directly which leads to better health in a short span.
With future research, the new delivery system could create a new type of delivery system for a wide spectrum of molecular treatments, including gene editing and substitution. Existing delivery devices for these therapies can be ineffective and randomly incorporate into cells’ genomes, and some can even trigger undesired immunological reactions. SEND holds the potential to circumvent these restrictions, thus opening up new avenues for molecular therapy deployment.
“The community of biomedical has been producing effective molecular therapeutics, but producing them to molecules in an accurate and efficient manner is difficult,” said CRISPR pioneer Feng Zhang, senior author on the study, Broad Institute core institute member, McGovern Institute investigator, and James and Patricia Poitras Professor of Neuroscience at MIT.
“He believes SEND can tackle these obstacles.” Zhang is a professor in MIT’s Departments of Brain and Cognitive Sciences and Biological Engineering, as well as a Howard Hughes Medical Institute scientist.
The team outlines how SEND uses molecules generated by human cells. PEG10, a protein that ordinarily attaches to its mRNA and makes a spherical protective cocoon around it, is at the heart of SEND. The researchers used PEG10 to package and transport additional RNA precisely in their investigation. SEND was used to transport the CRISPR-Cas9 genomic sequencing system in human and mouse cells, allowing them to modify specific genes.
PEG10’s ability to export RNA isn’t really unique, according to first author Michael Segel, a postdoctoral researcher in Zhang’s lab, and second author Blake Lash, a graduate. “That’s what makes it so thrilling,” Segel remarked.
“This research suggests that the human body may have alternative RNA transfer channels that can be used for therapeutic purposes. Also, it generates some interesting issues regarding how those proteins’ original functions might be.” The PEG10 protein is found in humans and is generated from a “retrotransposon,” a virus-like gene element that inserted itself millions of years ago into the genome of our forefathers.
Researchers discovered 4 years ago that ARC, a retrotransposon-derived protein, creates virus-like entities and is engaged in RNA transmission across cells. Despite the fact that these results revealed that retrotransposon proteins may be used as a delivery system, scientists had yet to properly pack and transport particular RNA payloads in mammalian cells.
Zhang’s team moved to retrotransposon-derived proteins as viable delivery vehicles after learning that some of these proteins can bind and pack genetic cargo. They went through the human gene looking for proteins that might construct protective shells in a methodical way.
A modular system has been designed which could be utilized to address medications for particular organs and tissues. The “SEND” protein, that is found in the PEG10 capsule, is the foundation of the SEND system. It will give a modular framework for designing disease therapies by mixing and combining various components.