Patients with resistant or relapsed acute myeloid leukemia (AML), a highly aggressive cancer, benefited from high-dose cytarabine followed by immunotherapy treatment with pembrolizumab, according to a clinical trial conducted at UNC Lineberger Comprehensive Cancer Center and Johns Hopkins Sidney Kimmel Comprehensive Cancer Center.
In the phase II trial, 37 patients under the age of 70 were enrolled. They were given high-dose cytarabine injections followed by intravenous pembrolizumab two weeks later to see if the inclusion of pembrolizumab enhanced clinical responses.
Immunotherapy Following High-Dose Chemotherapy Improves Prognosis Of Acute Myeloid Leukaemia
14 patients (38 percent) got complete remission of their cancer at the trial’s primary outcome. The research was conducted by cancer specialists, researchers, and experts to understand the effects of higher doses of Chemo on patients who have received better immunotherapy and to note their prognosis against the further development of the disease over a period.
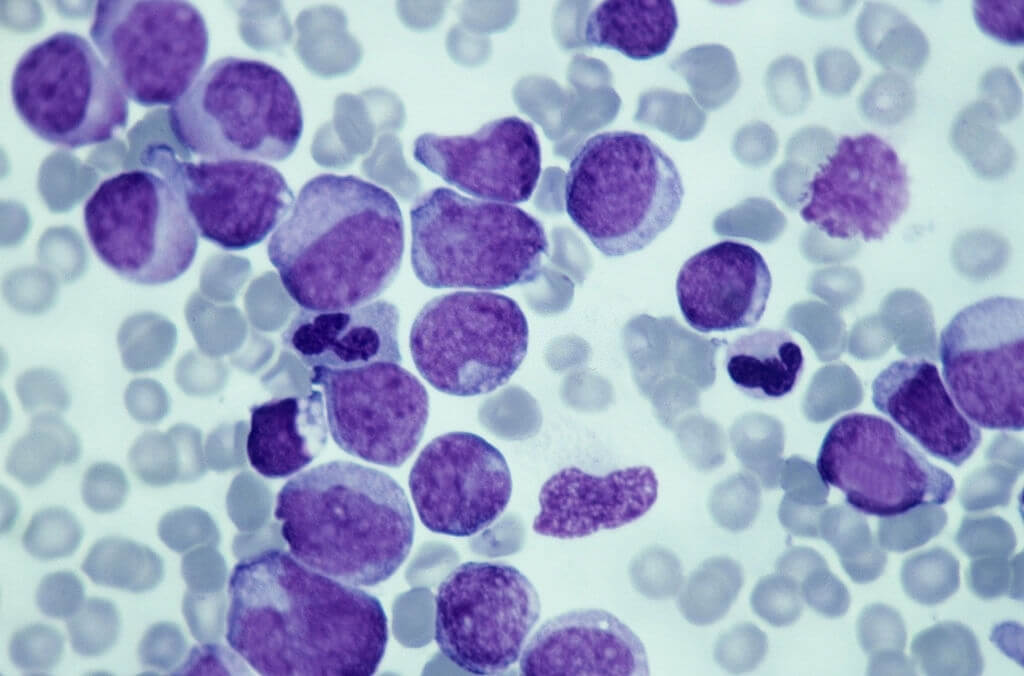
In refractory or relapsed AML, these results compare favorably to remission rates found with high-dose cytarabine and other chemotherapy regimens.
Even better, 46 percent of trial enrollees who had not responded to standard therapy and were given high-dose cytarabine followed by pembrolizumab in their second overall treatment phase achieved complete remission, indicating that this treatment may be most effective early in the course of their disease.
Serious adverse effects were uncommon and minor. “Despite extensive proof indicating immunotherapy may be helpful, AML has lagged behind other cancers, Research Center, and corresponding authorities.
“This is the first clinical trial to look at pembrolizumab in combination with intensive chemotherapy in patients with AML who have relapsed or become resistant to treatment,” says the researcher.
While five-year survival rates for AML have increased from about 6% in 1975 to about 30% now, survival rates in advanced stages of the disease remain dismal.
Patients whose cancer does not respond to vigorous treatment or develops resistance to chemotherapy have life expectancies measured in months, necessitating the quest for better medicines.
Overall, trial participants lived for over a year after receiving treatment, which is noteworthy when compared to past advantages seen with chemotherapy alone, which resulted in median survival of six to seven months.
The clinicians discovered that a specific type of immune-system cell known as a T cell was prominent prior to treatment, in addition to showing benefit for chemotherapy followed by immunotherapy.
The benefit of treatment was related to the function of these T cells, as pembrolizumab was able to revitalize a subset of T cells. The existence of these T cells could help doctors identify which individuals will benefit from pembrolizumab treatment for AML.
Different gene pathways were also more common in leukemia cells that responded to pembrolizumab, suggesting that these genes may be used as biomarkers to predict response.
The results of this trial demonstrate the potential of rationally designed combinations of cytotoxic chemotherapy with immune checkpoint blockade to treat histological cancers,” James Allison, Ph.D., who was awarded the Nobel Prize in 2018 for his research harnessing the immune system to attack cancer, and three colleagues from the University of Texas MD Anderson Cancer Center had high knowledge about this field.
While the combination appears to be beneficial (shifting the survival curve to the right in historical comparisons), long-term sustained results similar to those seen in other indications are still needed to bring checkpoint.
The clinicians discovered that a specific type of immune-system cell known as a T cell was prominent prior to treatment, in addition to showing benefit for chemotherapy followed by immunotherapy. The benefit of treatment was related to the function of these T cells, as pembrolizumab was able to revitalize a subset of T cells.