Vitamin A is given to the immune system to treat or prevent disease. Immunologists and geneticists at the University of Texas Southwestern Medical Center have uncovered how vitamin A enters immune cells in the intestines, results that could help cure digestive problems and possibly boost vaccine efficacy.
To date, we know that vitamins and protein are necessary for the well-being of the body, and in case of lack of any of them, there may be serious consequences.
Scientists Have Now Discovered How Vitamin A Enters The Gut’s Immune Cells
Research has made experts look more into the presence and role of Vitamin A in the human body recently, showing the better results have an effect on guts.
Vitamin A—is a fat-soluble nutrient that the body converts to retinol and then to retinoic acid before it can be used—is essential for every tissue in the body. It’s especially important for the adaptive immune system, a subset of the larger immune system that reacts to specific pathogens based on immunological memory, established through disease or vaccination exposure.
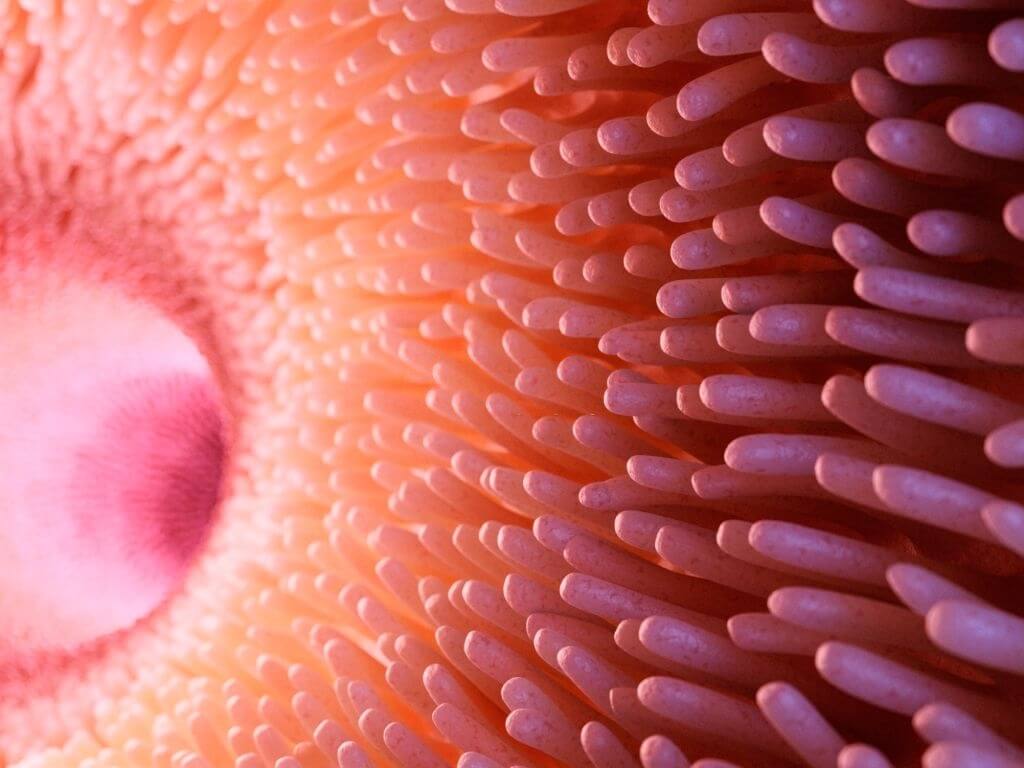
Although it was known that some intestinal immune cells called myeloid cells could convert retinol to retinoic acid, the source of retinol for this task was unknown; researchers discovered that resident intestinal bacteria have an impact on the biology of humans and other animal hosts.
Amyloid in the blood, some organs create proteins, a family of retinol-binding proteins when they are infected. They identified LDL receptor-related proteins using biochemical techniques to determine which cell surface proteins they linked to.
Joachim Herz, M.D., Director of the Center for Translational Neurodegeneration Research and Professor of Molecular Genetics, Neurology, and Neuroscience at UT Southwestern discovered LRP1 more than 30 years ago. The Herz lab studies the molecular processes by which members of the LDL receptor gene family act in the brain and vascular wall as signaling and endocytic receptors.
The LDL receptor was discovered at UT Southwestern, which helped Michael Brown, M.D., and Joseph Goldstein, M.D., won the Nobel Prize in Physiology or Medicine in 1985.
LRP1 was found on myeloid cells in the intestine, where it appeared to transport retinol. The adaptive immune system in mice’s gut was virtually eliminated when the researchers utilized genetic procedures to erase the gene for this receptor, preventing their myeloid cells from taking up the vitamin A derivative.
The bone marrow produces all innate immune cells, but they eventually spread throughout the body. Barrier tissues contain innate lymphoid cells, which comprise the group. While it is well known that innate lymphoid cells are concentrated in the intestines, how these cells get there has remained a mystery
Critical components of adaptive immunity, T and B cells, and the molecule immunoglobulin A, were severely diminished.
The researchers then evaluated the responses of mice with and without LRP1 to Salmonella infection. Those who did not have the receptor were immediately infected.
LRP1 appears to be the vehicle by which retinol penetrates myeloid cells, according to the findings reported in Science. If scientists can find a way to stop this process, it will be a huge breakthrough.
It also can reduce the immunological response in inflammatory bowel disease and Crohn’s disease, both of which impact the intestines. Finding a means to stimulate LRP1 activity, on the other hand, could boost immunological activity, making oral vaccinations more effective.
Within the immune system, two types of cells work together to rid the body of infection: innate immune cells, such as innate lymphoid cells and leukocytes, which act quickly to eliminate infection; and adaptive immune cells, such as T-cells and B-cells, which arrive later but are more effective at killing or neutralizing the pathogen.