IDO promotes suppressive components of the complements immunological systems in addition to activating tryptophan metabolism. As per Derek Wainwright, Ph.D., adjunct professor of Neurological Surgeons, and senior author of the paper, this discovery probably explains partly how therapeutic attempts in terminal malignancies like glioma had failed.
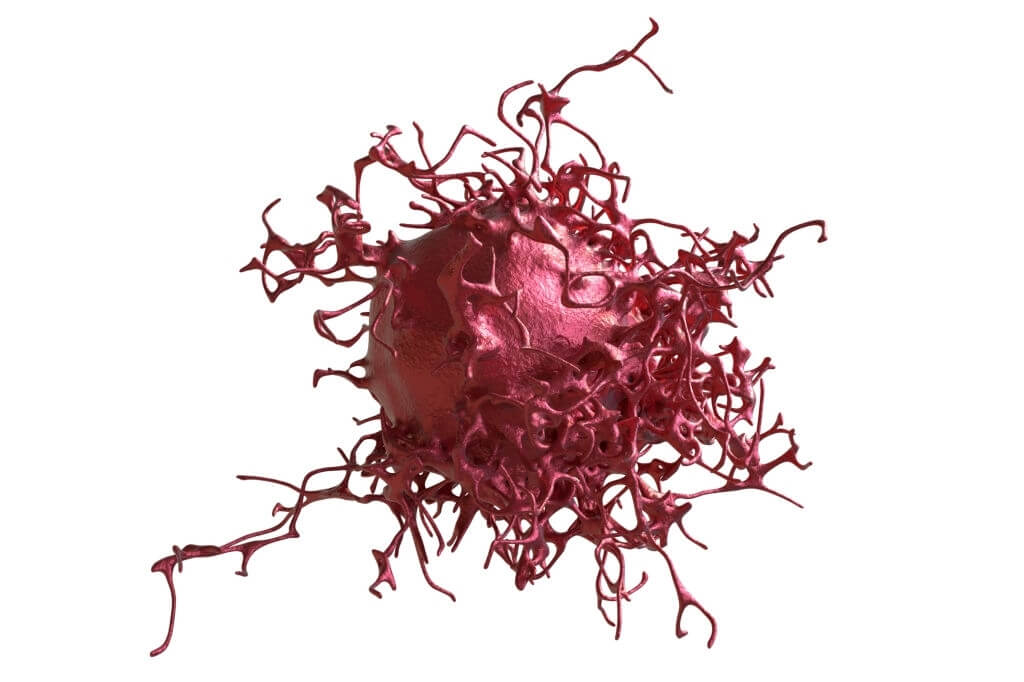
As per research released in Clinical Cancer Studies, most tumors create an enzyme known IDO that inhibits immunity systems function, however, the lengthy notion about how these process works have to be revised.
Rethinking Cancer-Induced Immunosuppression
To be sure about this, the experts have checked a variety of samples from different cases and regions. This has made them rule out probabilities of effects of any external factor and concentrate on the development of tumors within the body. This research has shed light on some additional facts that can help the experts decide a better option to help the patient.
Wainwright, a professor of Sociology in the Divisions of Hematology and Oncology and Microbiology-Immunology, said, “We have opened up new possibilities into understanding how IDO suppresses the anti-cancer immune response that is independent of its historical and predominant association with tryptophan metabolism.”
IDO activity is found in several tough malignancies, such as glioblastoma, prostate, and stomach cancer. The protein transforms serotonin, an essential nutrient that could solely be taken by food, into a molecule termed kynurenine. The traditional explanation for how IDO reduces the anti-tumor immune reaction predicated on Petri plate studies is the reduction of serotonin and the increase of hypoxanthine.
“For greater than 20 years, we have assumed this is how IDO affects the immune response,” Wainwright said.
Several medical studies combining therapy with pharmacological IDO cholinesterase inhibitors had unable to demonstrate a significant increase in overall mortality compared to treatment alone. As a result, Wainwright & his partners had to start over with IDO. In the latest study, researchers eliminated IDO in animals with tumors that were identical to glioblastoma, then revived IDO with either a normal version or a type that had no enzyme function.
One mechanism, in particular, drew their eye throughout their examination of IDO in tumor cells: the complements cascades. The complements cascades is an innate immune cells component in which hepatocytes inside the liver produce a complements component that attaches to intruders or inflammatory tissues to assist and neutralize a virus or injured tissue.
IDO also regulates complement factor H (CFH), which serves as a regulator of the complement system to avoid over of supplement defense towards foreign invaders. They discovered that IDO, irrespective of its capacity to metabolize tryptophan, is linked to reduced longevity and increased suppressive cell buildup in research rats with brain tumors.
As per Wainwright, CFH is a good focus for developing novel inhibitors that might be used in conjunction with therapy. To develop a new class of medicines, massive chemical-genetic screening was presently being used to find ligands that could attach to and suppress CFH.
“This system is poorly studied, and the association between IDO and CFH has never been discovered for any cancer before our study,” Wainwright said.
Removal or alteration of common-chain eicosanoids causes significant immunological abnormalities in humans and mice, which varies. This process, according to Wainwright, could be seen in other IDO-rich malignancies outside glioblastoma, such as the pancreas and colorectal cancers. Furthermore, in mouse models, mutations of critical signaling proteins in T cells have dramatically different effects.
As a result, we suggest developing a unifying model of tumor cell intricacy that takes into account species variations. To assess the degree to which study findings from the deficient mice could be extended to humans, we need to improve our immune monitoring techniques.