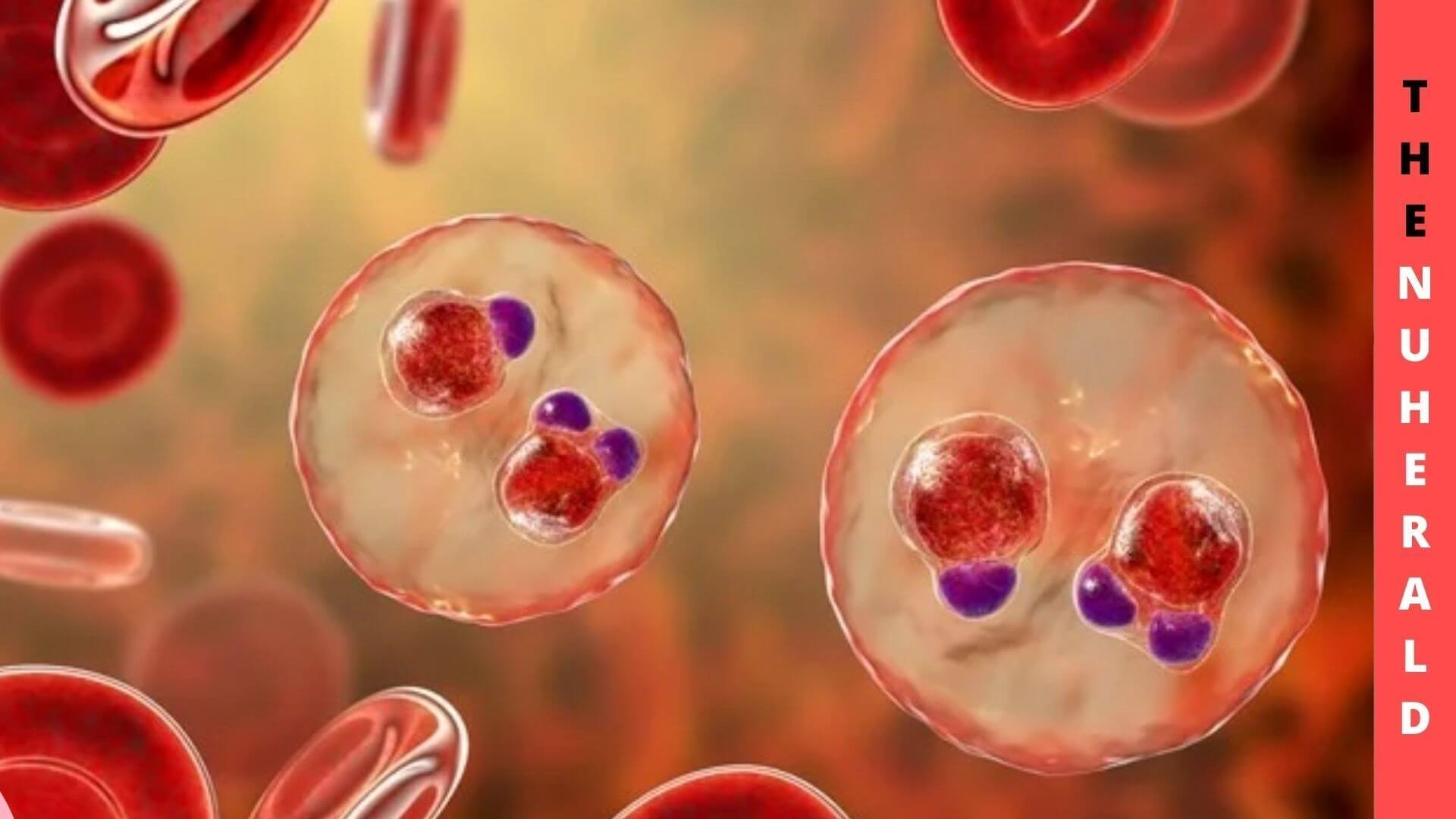
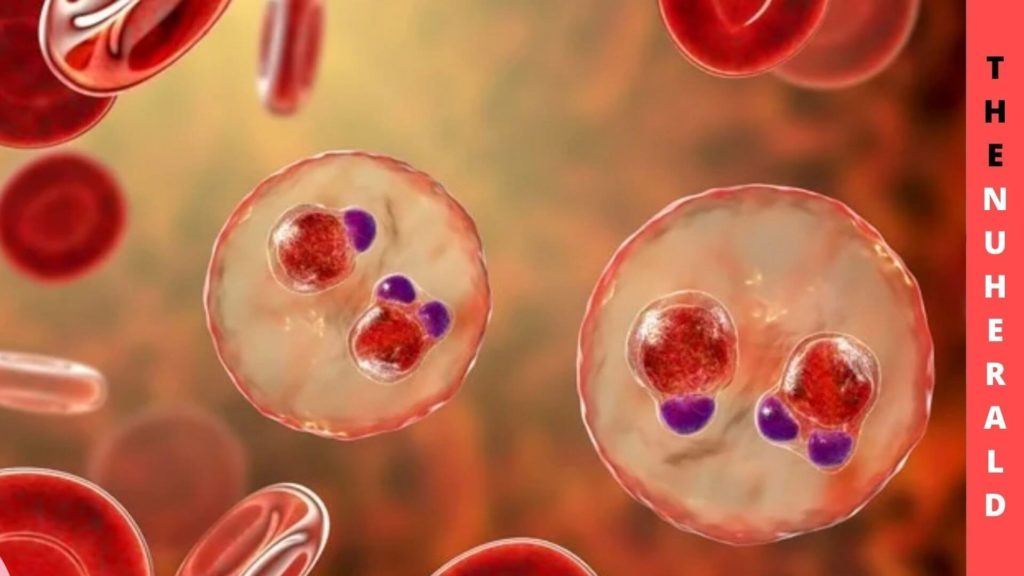
Malaria, particularly Plasmodium falciparum-caused dengue fever, was a significant source of illness and death through time; as a consequence, plasmodium seems to have placed extreme adaptive stress on the genetic code selecting for some genetic polymorphisms which guard against serious disease.
The Connection Between New Malaria Parasite & Sickle Hemoglobin
The most genetic variation linked to malaria causes brittle hemoglobin (HbS). The significant frequency of HbS in Sub-Saharan and other tropical places is likely due to heterozygotes’ resistance to malaria.
Since the preventive impact of sickle cell type on plasmodium was initially published over 60 years ago, our knowledge of the demography and mechanisms of preservation of these genotypes has grown as it will be explored more hereunder.
Notwithstanding the evident negative effects of HbSS, now it is commonly acknowledged that the hemoglobin mutation’s survival in populations is owing to heterozygous people’s immunity from malaria.
In 1949 Haldane suggested the idea of a heterozygosity edge in the fight against the disease. Haldane proposed in this important study that those who are heterozygous with β – thalassemia, additional hemoglobinopathy, are immune from malaria.
When opposed to HbAA people, higher peroxidation and clearing of parasitoids HbAS red blood platelets by the splenic can contribute to greater innate immunity and faster establishment of protective immunity. Throughout normal times and plasmodium, cross-sectional research observed lower levels of peripheral monocyte oligodendrocytes and monocytes in people with HbAS implying greater monocytes and dendritic cell migration to the splenic.
Professor David Conway, the study’s lead author and a biology professor at LSHTM, said: “Making the connection between the genetic variants of the parasite and its ability to infect those with sickle hemoglobin paves the way for research to dive deeper into the biological mechanisms behind this.
Greater clarity on the ways that P. falciparum evades the human body’s defenses could lead to new opportunities for protecting against malaria and treating those living in the most affected areas.”
Several chemical and immunological processes are expected to play a role in the HbAS genotype’s resistance against falciparum malaria. HbS causes biochemical changes in red blood cells, which may impact parasite metabolism and proliferation. Plasmodium falciparum causes oxidative damage to HbAS red blood cells as well. In sickled blood cells, persistent low concentrations of oxidized haem may produce HO-1 resulting in human resistance in serious infection.
The creation of a cytoskeletal may be hampered by oxidized haem alternations of PfEMP-1 with the expression on the contaminated red blood cell surface and decreased cytoadherence.
According to Dr. Gavin Band: “We have known for years that human genetic variants such as sickle hemoglobin can protect against malaria, but we wanted to understand if malaria parasites have evolved to overcome this. In our study, large-scale genome sequencing allowed us to compare thousands of human and parasite genomes.
For the first time, we were able to highlight a correlation between the human sickle hemoglobin mutation and three regions of the parasite genome, suggesting that the human genome is a selective pressure in the evolution of the parasite.”
Enhanced activation of specific in the spleen may hasten the formation of protective immunological responses such as antibodies to PfEMP-1, which could be boosted by chemical defense from excessive parasite concentrations, which could otherwise suppress an effective response.
Antibodies targeted towards PfEMP-1 and probably additional membrane proteins may accelerate complement activation and ingestion of contaminated red blood cells as well as further disrupt their cytoadherence capabilities.
Although there is evidence for all of these pathways, it is uncertain whether one is important in vivo. Nevertheless, related pathways contribute to superior taking full advantage of control and protection both against simple and serious malaria in HbAS children. The host-parasite connection, particularly how Plasmodium falciparum interacts with human immune systems, would benefit from a better knowledge of the mechanism of resistance generated from this single data point alteration.